I'm Rachael
Mom of 3 & Baby Sleep Expert with Big Sis Energy
& I’VE DONE ALL THE RESEARCH FOR YOU ALREADY.
Better sleep for the entire family
BROWSE COURSES
hey!
when does a baby stop eating at night?
Many parents want to know if their baby is actually hungry at night, and if they should be getting fed overnight at a certain age. Many pediatricians and other healthcare professionals will tell parents that their baby shouldn’t need nighttime feedings by certain arbitrary ages or weights.
The truth is that feeding throughout the night IS normal, and depending on the mother/baby dyad, night feeds might last well into the first year and beyond. Babies’ tummies are tiny and they can only hold so much breastmilk or formula at a time. Because of this, they often need to be fed every few hours throughout infancy, which of course causes them to wake up hungry in the middle of the night (often multiple times). As they grow their stomach capacity grows as well, and many babies are able to sleep through the night without feedings at a few months of age. However, just because some babies CAN sleep through, doesn’t mean they all do or should. Every baby is different!
Only about half, or approximately 57% of 12-month olds “sleep through the night”, with SSTN defined as just an 8-hour stretch at any point in the night. For context, this might mean that a baby who goes to bed at 7:00pm would wake up and need you at around 3:00am at best. I know it may seem like everybody else’s baby sleeps through and doesn’t feed overnight anymore, but the research says otherwise!

Let’s take a look at some more research on baby sleep and feeding to find out what’s normal and what you can expect for feeding at night.
-
One study took 715 mothers with babies 6-12 months old. They found that “78.6% still regularly woke at least once a night, with 61.4% receiving one or more milk feeds. Both night wakings and night feeds decreased with age. No difference in night wakings or night feeds was found between mothers who were currently breastfeeding or formula feeding. However, infants who received more milk or solid feeds during the day were less likely to feed at night but not less likely to wake.” (Brown & Harries 2015).
-
Another study looked at the total amount of breastfeeds per 24 hours for infants 1-6 months. It found that night breastfeedings were common and made an important contribution to the total milk intake. Infants breastfed 11 +/- 3 times in 24 hours (range: 6-18) (Kent et al 2016).
-
Another study which didn’t look at feeding in particular but at night wakings found that, using a definition of either 6 or 8 hours of uninterrupted sleep, 27.9% to 57.0% of 6- and 12-month-old infants did not sleep through the night. We can only assume that many of those infants were waking up and using a feeding to get back to sleep (Pennestri 2018), as this is often the quickest and easiest way to soothe babies at night.
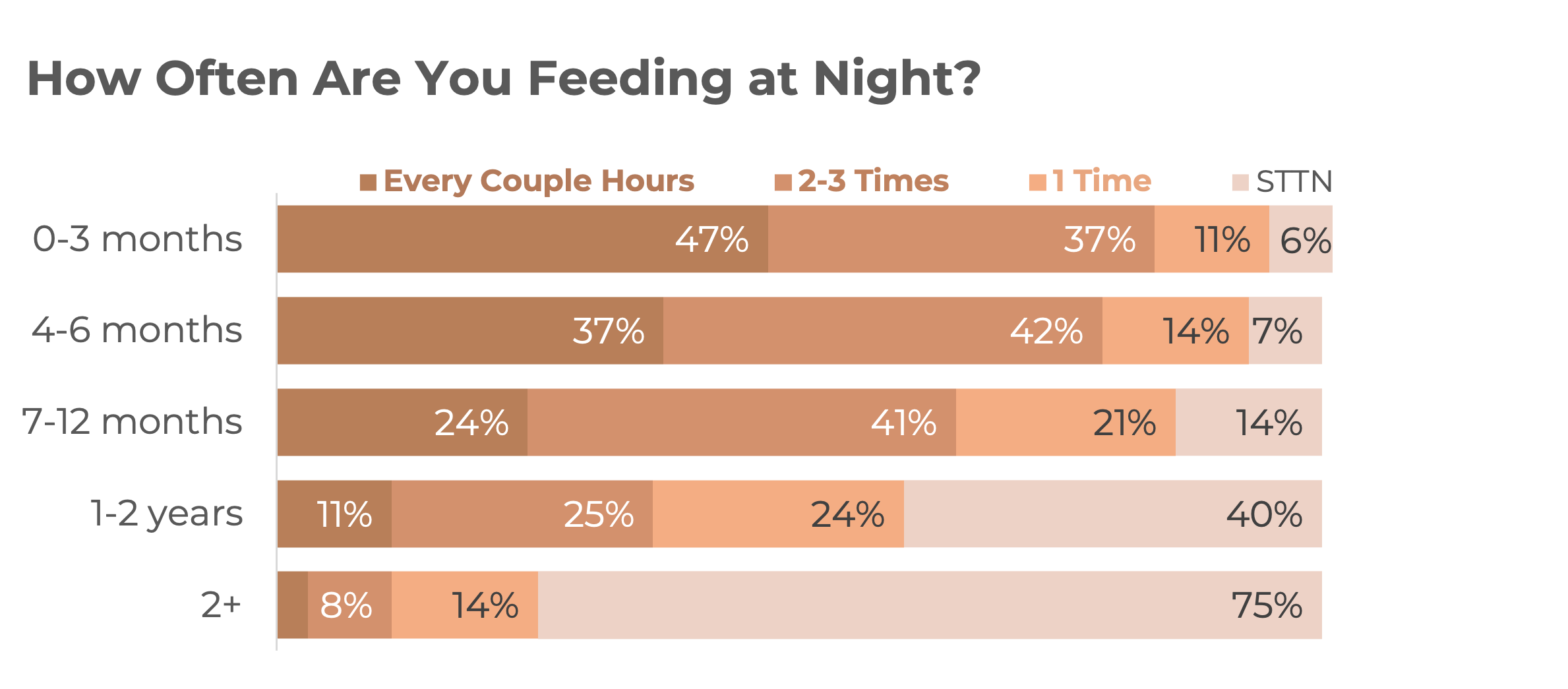
I also asked in my stories, and here’s what the HSB Instagram community said:
When your baby isn’t yet sleeping through the night and is waking for multiple feedings, there are a few things to consider:

-
Daytime feeds. Is your baby getting enough milk feedings (plus solids if 6+ months) during the day? You can use this milk calculator to determine about how much milk your baby should need by age per day. At 6-7 months you can add in 1-2 “meals” of solids per day. Solid Starts is a phenomenal resource for figuring out your child’s dietary needs, and they have a breakdown by age here for milk, meals, and snacks. Ensuring adequate daytime nutrition could get you longer stretches of overnight sleep if your little one is waking due to hunger. One thing you can try if the night feeds seem excessive is to add in one extra breastfeeding session or bottle during the daytime.
-
Full feedings. When your baby wakes for a feeding at night, are they latching on and then falling back to sleep within just a couple of minutes? This means they aren’t really taking a full feeding. It’s natural for them to be sleepy at the breast, but that doesn’t mean they’re full! Try to keep them awake enough to take a “full” feeding, whatever that normally is for them. This will ensure that they are in fact satisfied and won’t wake due to hunger again at the end of the next sleep cycle or get into a snacking all night pattern! The brain regards hunger as a top priority to be met, so it’s not very easy to fall asleep or STAY asleep if not satiated.
-
Sleep Associations. Up until at least 6 months you can pretty much depend on your baby needing to feed at least a couple of times per night. After that is when some babies are able to go longer stretches or even all night without feedings. Now if your little one is over 6 months and you’re confident that they aren’t actually waking up from hunger, you could try adding in some other sleep associations for them. It might be that they wake up for a reason besides hunger (needing comfort, thirst, cold, etc.) but still rely on sucking or feeding to get back to sleep. If they’ve just eaten and/or you’re sure they don’t actually need to be fed, you can try other methods of soothing them back to sleep.
-
Ruling out red flags. If your little one is struggling with feeding, uncomfortable, or showing other signs that seem “off” to you, check out this blog post on red flags for baby sleep.
A Quick note on breastmilk vs. formula:
It’s commonly thought that formula may help babies sleep better at night. Some parents think that “topping off” with formula or switching to formula from breastmilk may be the answer to their sleep issues. This isn’t supported by the research. Breast milk contains natural sleep-inducing hormones such as melatonin, tryptophan, and serotonin that can help babies fall asleep faster and stay asleep longer. A study published in the Journal of Perinatal Education found that breastfeeding mothers reported fewer night awakenings and less overall sleep disturbance than formula-feeding mothers.
Additionally, a systematic review published in the Journal of Human Lactation found that skin-to-skin contact during breastfeeding is associated with increased sleep duration and better sleep patterns for infants. Another study published in the Journal of Human Lactation found that infants who were bottle-fed experienced more sleep disruption and less total sleep time than breastfed infants.
Of course however you feed your baby is completely up to you, but don’t believe the myth that introducing formula will get you better sleep!

“When Can I Stop Feeding at Night?”
After 12 months of age, solid foods start to replace breastmilk or formula as the main source of your baby’s nutrition. This means that after age 12 months you may consider parent-led night weaning. Of course many babies also self-wean as they begin to sleep longer and longer stretches on their own- so initiating weaning may not be necessary for you!
To begin the weaning process you’ll want to first ensure proper daytime nutrition, set up boundaries with your child, and figure out alternative comforting strategies or enlist your partner to respond to night wakings. It’s usually advised to cut one feeding at a time rather than cold turkey, both for your baby’s sake and for your comfort.
Weaning post 18 months tends to be the easiest time, as your toddler will have more language and understanding. Check out the HSB Night Weaning Workshop here if you’re looking to cut out night feedings or to stop feeding your baby or toddler to sleep.
What about weaning your baby from bottle feeds?

A lot of the information in this post relates to breastfeeding but can be applied to bottle weaning as well. Here are some things that are the same no matter if baby is breast or bottle fed.
Up to 12 months, a baby’s primary source of nutrition is breastmilk or formula even if they’ve been well established on solids.
To begin weaning from either day OR night feeds, there are only a couple of options: reduce either the number or length/ounces of feedings.
Here’s what’s a little different about formula weaning and some ideas for you:
It’s generally recommended to start weaning your baby off the bottle between 12 and 24 months of age and immediately start using a cup instead (per the AAP), mainly due to risks of tooth decay and obesity.
You can start with gradually reducing the amount in each bottle. If you usually offer your child 6 ounce bottles, offer only 4 ounce bottles for a few days, then reduce a little bit more until it’s gone. If you’re concerned with your child’s calorie intake, you can offer the remaining 2 ounces from a cup.
You can also reduce the number of bottles offered. If there’s no concern with baby’s weight, you might choose to just remove one bottle that’s normally offered in the night, and offer your child some water and other comforts like rocking, a cuddle or a back rub.
If your little one is having a hard time letting go of the bottle, you could try diluting the milk with water more and more over a couple of weeks. They will likely lose interest when the bottle is mostly water. *NOT appropriate for <12 months*
If your baby only takes one bottle at night, you might decide to just lose it cold turkey and offer water and cuddles to get back to sleep instead, and be sure baby gets plenty to eat during the day.
How do you know you’re ready to night wean your baby or toddler?
This is a very personal choice that every parent makes at a little bit of a different time. For some, baby decides when to wean and the parents don’t get a choice at all! For others, some parent-led changes and gentle nudging is needed to wean one or all nighttime feeds. Before you decide to start weaning, it’s a good idea to consider and reflect on the following first!
-
Is your baby at least 12 months old?
-
Is your baby teething or sick, or going through any other big change right now?
-
Is your baby highly sensitive? Are you or your partner highly sensitive? Do you have coping techniques in mind in case some nights are really tough?
-
Are there any issues with feeding, weight gain or other health concerns for your baby?
-
Would you like to continue breastfeeding for some night feeds/ during the day? Do you have an idea about how you might set boundaries around this with your child?
-
Are you resenting feedings at night? Are you feeling increasingly more touched out, or do you have anger or aversion toward breastfeeding?
-
Do you bed share/ room share and if so, do you want this to continue or do you want to make a change in your sleep arrangement first?
-
Are there any issues/ concerns with latch, supply, etc. or a history of mastitis for the breastfeeding parent?
-
Are you pregnant, trying to conceive or wanting to get your cycle back?
-
Are you using weaning as a desperate attempt at better sleep? Have you ruled out potential red flags that could be causing more-than-normal waking first?
Inside the Night Weaning Workshop you’ll get to work through all of these questions and more. By the end, you’ll have a confident mindset and strategy to begin your night weaning journey when you’re ready.

Featured
When daylight saving time ends, we “fall back” one hour, meaning that sunrise and sunset will occur an hour earlier. How will this affect your baby’s sleep?
Responsive sleep tips and support for parents of multiples or twins.
What are floor beds? When to use them? And How to use them?
Before you start changing anything it’s important that you have ruled out any underlying reasons why your infant might have such a strong link to staying latched.
Between the ages of 2-3, many toddlers will experience a heightened level of fear and anxiety. They go through a big developmental leap in their imagination but their ability to distinguish between reality and fantasy doesn’t quite match up! Cue the sudden influx of questions about monsters…
Here are my best tips and tricks to help you bridge this transition. I found that I needed to prepare myself as a mom and prepare my baby. So here are my practical tips for preparing the YOU!
Here are my best tips and tricks to help you bridge this transition. I found that I needed to prepare myself as a mom and prepare my baby. So here are my practical tips for preparing the YOU!
Most parents get to a point where their current method of supporting baby’s sleep stops working. Perhaps you want to switch things up in your bedtime routine, or you want to change what you use to help your baby to sleep. Whatever your reason for wanting to change up the sleep associations, these are my quick tips for making gentle changes without any need for sleep training.
‘How can I involve my partner in my baby or toddler’s sleep?’ Perhaps you want to more evenly share the load of navigating the world of baby or toddler sleep, or your baby is no longer falling asleep at the breast and you want your partner to be able to put them down for sleep, or you have a second child and you want to divide bedtimes.
It’s true that “sleep regressions” aren’t really a thing but that you may notice sleep backslide during big periods of development. And the 18 month mark definitely fits the bill! There may be some changes to sleep around this age and you may notice increased difficulty with getting your toddler down for naps or nights.
Bedtime can be a challenging time for both children and parents, especially when toddlers and young children have difficulty falling asleep. Many factors contribute to this common bedtime struggle, leaving parents wondering how to create a peaceful and restful sleep routine without resorting to sleep training methods. In this blog post, we will delve into why it might take a toddler or young child a long time to fall asleep at bedtime and explore various strategies parents can try to help their little ones settle into a peaceful slumber without sleep training.
Sources:
-
Feldman-Winter L, Goldsmith JP. Evidence-Based Policies and Practices for Breastfeeding and Sleep. J Hum Lact. 2016;32(3):446-455. doi:10.1177/0890334416648002
-
Tikotzky L, Glickman-Gavrieli T. Sleep and feeding interactions in infants: a review. Infant Behav Dev. 2017;49:120-128. doi:10.1016/j.infbeh.2017.07.008
-
Mindell JA, Li AM, Sadeh A, Kwon R, Goh DY. Bedtime routines for young children: a dose-dependent association with sleep outcomes. Sleep. 2015;38(5):717-722. doi:10.5665/sleep.4680
-
Pinilla T, Birch LL. Help me make it through the night: behavioral entrainment of breast-fed infants’ sleep patterns. Pediatrics. 1993;91(2):436-444. PMID:8424017
-
Cohen Engler A, Hadash A, Shehadeh N. Breastfeeding may improve nocturnal sleep and reduce infantile colic: Potential role of breast milk melatonin. Eur J Pediatr. 2012;171(4):729-732. doi:10.1007/s00431-011-1659-1
-
Sadeh A, Anders TF. Infant sleep problems: origins, assessment, interventions. New York, NY: Guilford Press; 1993.
-
Adams EJ, Palombini L, Sipsma HL, et al. A qualitative exploration of infant feeding decision-making for first-time mothers experiencing breastfeeding difficulties. Matern Child Nutr. 2019;15(4):e12808. doi:10.1111/mcn.12808
-
Doan T, Gardiner A, Gay CL, Lee KA. Breast-feeding increases sleep duration of new parents. J Perinat Educ. 2007;16(4):35-41. doi:10.1624/105812407X244768
-
Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breastfeed Med. 2015 Jun;10(5):246-52. doi: 10.1089/bfm.2014.0153. Epub 2015 May 14. PMID: 25973527.
-
Kent JC, Mitoulas LR, Cregan MD, Ramsay DT, Doherty DA, Hartmann PE. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006 Mar;117(3):e387-95. doi: 10.1542/peds.2005-1417. PMID: 16510619.’
-
Pennestri MH, Laganière C, Bouvette-Turcot AA, Pokhvisneva I, Steiner M, Meaney MJ, Gaudreau H; Mavan Research Team. Uninterrupted Infant Sleep, Development, and Maternal Mood. Pediatrics. 2018 Dec;142(6):e20174330. doi: 10.1542/peds.2017-4330. Epub 2018 Nov 12. PMID: 30420470.
Was this helpful? Save it for later!

binge reads
We think you'll love these
You deserve to the
baby stage, not just "survive it."
And you DON'T have to sacrifice your values, ignore your instincts, or force yourself to follow a method you don't align with just to get your baby back to sleep.
I’m here to help you create a restful, sustainable sleep environment that honors both your baby’s needs AND your own (without the stress OR the guilt!) because, no, you don’t have to choose between the two.
enjoy!
BABY SLEEP COURSES →
BABY SLEEP CONSULTS →
Wish you could help your baby sleep better without resorting to sleep training? Download my FREE guide to a good night’s sleep and learn 8 simple, science-backed tips for supporting your child’s needs.
Traditional sleep training methods don’t have to be your solution to better sleep.
SLEEP TRAINING ISN’T THE ONLY WAY TO GET GOOD SLEEP
Hey, I'm Rachael and Hey, Sleepy Baby is for parents who want to get their nights back, without sleep training their babies.
NO ONE TOLD US POD
explorING the untold truths of parenting














